

High heels have long been a symbol of fashion and elegance, worn by millions of women around the world. However, while they may enhance your outfit and boost your confidence, there is a downside to wearing high heels too often. Many women experience lower back pain, achy hips, and tightness in the leg muscles as a result of wearing high heels. In this comprehensive guide, we will explore the impact of wearing high heels on your back and discuss ways to relieve back pain and prevent injury.
The Effect of Wearing High Heels on your Back
When you slip on a pair of high heels, you may not realize the toll it takes on your back. High heels can alter the natural alignment of your spine, putting you at risk for back pain. The spine is made up of vertebrae stacked on top of each other, with jelly-filled discs that act as cushions between them. Its natural shape is a gentle S-curve that allows for smooth movement and supports the entire body evenly.
However, when you wear high heels, the alignment of your spine is compromised. The body tries to compensate for the imbalance by bending or flexing the spine and hips, tensing the muscles of the calves, hips, and back. This can lead to fatigue, strain, and uneven wear and tear on the ligaments, joints, and vertebral discs of the back.
Reasons Why High Heels Are Bad For Your Back
Spinal Injuries that May Result from wearing High Heels
Wearing high heels regularly can have long-term effects on your back and spine. Here are some of the spinal injuries that may result from wearing high heels:
High Heels Can Cause Strains and Sprains in the Back and Feet
Wearing high heels can lead to strains and sprains in the back and feet. There are two primary reasons for this:
Another reason why high heels can cause back pain is the effect they have on posture. The altered alignment of the spine caused by high heels can lead to a forward head posture and rounded shoulders. This can put additional stress on the back, leading to muscle imbalances and potential pain.
High Heels can Increase the Risk for Back Pain - Here's how
The combination of the altered alignment of the spine, tightened muscles, and changes in posture due to wearing high heels can increase the risk of back pain. The strain on the back, hips, and legs can result in discomfort and potential long-term damage to the spine and surrounding structures.
Reasons Why You Shouldn't wear Heels everyday
While high heels may be fashionable, it's important to consider the potential risks and limitations associated with wearing them every day. Here are some reasons why you should avoid wearing heels regularly:
What Can You Do to Relieve Back Pain and Prevent Injury?
If you experience back pain from wearing high heels, there are steps you can take to relieve the pain and prevent further injury. Here are some tips:
How can I save my back from wearing heels?
What exercises can I do to prevent and relieve back pain from wearing heels?
Remember, if you have suffered from a serious back injury or chronic back pain, it is essential to seek professional medical advice and treatment options. A qualified healthcare provider can assess your condition and provide appropriate guidance.
In conclusion, while high heels may be a fashion statement, wearing them too often can lead to back pain and potential long-term damage. It is important to be mindful of the impact high heels can have on your spine and take steps to relieve back pain and prevent injury. By choosing lower heels, wearing properly fitted shoes, and incorporating stretching and strengthening exercises into your routine, you can minimize the risks associated with wearing high heels. Your back will thank you for it!
For more information about relieving back pain and preventing injury, contact Achilles Foot Clinic, a leading Podiatry Clinic based in Calgary, AB.
Plantar fasciitis is a common condition that affects the foot, specifically the plantar fascia, a tissue that connects the toes to the heel bone. It is characterized by heel pain, inflammation, and tenderness. However, many people wonder if plantar fasciitis can cause calf pain or if it is related to pain in other parts of the leg. In this article, we will explore the relationship between plantar fasciitis and calf pain, as well as other leg pain symptoms. We will also discuss the causes, symptoms, and treatment options for plantar fasciitis.
What is Plantar Fasciitis?
Plantar fasciitis is a condition that occurs when the plantar fascia, a thick band of tissue that runs along the bottom of the foot, becomes inflamed or irritated. This can happen due to activities that put stress on the foot, such as running, standing for long periods, or wearing improper footwear. The pain is typically felt in the heel and is often described as a stabbing or sharp sensation.
Does Plantar Fasciitis Really Cause Calf Pain?
While calf pain is not a direct symptom of plantar fasciitis, there is a relationship between the two. The pain from plantar fasciitis can alter the way a person walks, leading to compensatory movements and strain on other parts of the leg, including the calf. This can result in calf pain or tightness. However, it's essential to note that the calf pain is a secondary symptom, caused by the altered gait pattern rather than the plantar fasciitis itself.
Does Plantar Fasciitis Cause Your Whole Leg to Feel Pain?
In some cases, the pain from plantar fasciitis can radiate to other parts of the leg, including the ankle, knee, hip, or back. This is because the altered gait pattern can affect the muscles, ligaments, or joints in the rest of the leg, leading to pain in those areas. However, it's important to differentiate between referred pain from plantar fasciitis and pain originating from other sources. If the pain in the leg started before the foot pain, it may not be plantar fasciitis but rather referred pain from a different part of the body.
Can Plantar Fasciitis Cause Ankle Swelling?
No, plantar fasciitis does not typically cause ankle swelling. Swelling around the ankle is more likely to come from issues related to the ankle joint or tendons crossing it. For example, the tibialis posterior tendon can cause swelling on the inside of the ankle, which may feel similar to plantar fasciitis when injured near its attachment under the foot. Therefore, if you experience ankle swelling along with foot pain, it's important to consult a healthcare professional to determine the underlying cause.
Can Plantar Fasciitis Cause Swelling at the Top of the Foot?
No, plantar fasciitis does not cause swelling at the top of the foot. Swelling on top of the foot is more likely to be due to issues with the little joints, bones (such as stress fractures), or tendons (such as tenosynovitis) on top of the foot. If you notice swelling in this area, it's important to seek medical attention to determine the cause and appropriate treatment.
Some Conditions That Are Often Misdiagnosed as Plantar Fasciitis
Plantar fasciitis can sometimes be misdiagnosed as other conditions that cause foot pain. Here are a few conditions that can be mistaken for plantar fasciitis:
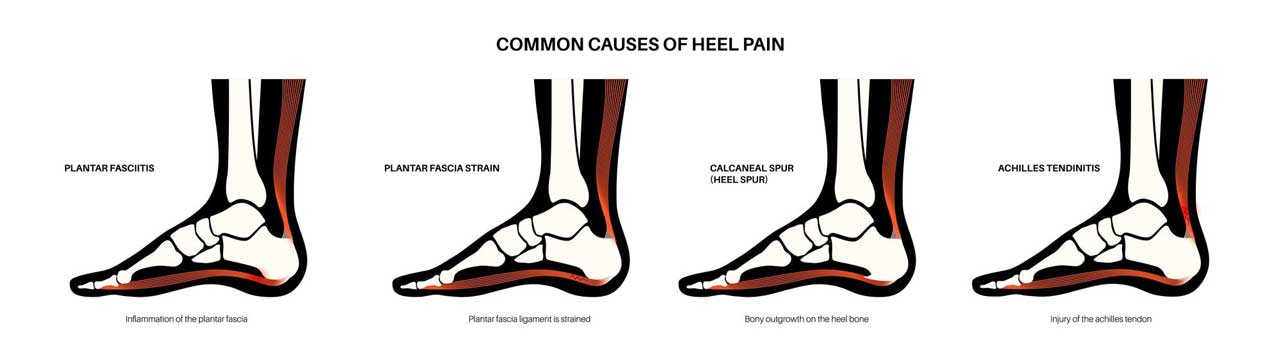
Heel Spur Syndrome
Heel spur syndrome is often used interchangeably with plantar fasciitis to describe the same condition. It is characterized by the presence of a bony growth (heel spur) on the heel bone. However, researchers suggest that these terms are too simplistic and that the term "plantar heel pain" should be used instead, as there are often multiple factors contributing to the pain. Imaging studies often reveal a combination of factors, including bone edema, changes to the heel fat pad, injuries to the plantar fascia, and heel spurs.
Stress Fracture
Calcaneal (heel bone) stress fractures can cause pain that is similar to plantar fasciitis. These fractures are often seen in endurance athletes with a pronounced heel-strike running style or in military recruits. However, stress fractures can also occur in individuals with low bone density (osteoporosis) without any specific physical activity. Differentiating between stress fractures and plantar fasciitis can be challenging, and an MRI scan is often necessary for an accurate diagnosis.
Achilles Tendonitis
Achilles tendonitis is a condition characterized by inflammation of the Achilles tendon, which connects the calf muscles to the heel bone. It can cause pain in the back of the heel and along the tendon. It's important to distinguish between plantar fasciitis and Achilles tendonitis based on the location of the pain. If the pain is felt on the Achilles tendon or at its attachment to the heel bone, it is likely Achilles tendonitis and not plantar fasciitis. On the other hand, if the pain is felt under the foot, close to the inner part of the heel bone, it is likely plantar fasciitis.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition caused by compression or irritation of the tibial nerve as it runs around the inner part of the ankle. This can result in pain and other sensations, such as burning, electric shocks, pins and needles, or itching. The pain can be similar in location to plantar fasciitis, but it is usually described differently. Plantar fasciitis pain is often described as tightness, an ache, or sharp pain, while tarsal tunnel syndrome pain may be more widespread under the foot or close to the bone on the inside of the ankle.
Heel Fat Pad Syndrome
Heel fat pad syndrome refers to pain caused by the bruising or thinning of the fat pad under the heel. This can result in pain under the heel, especially when pressure is applied. Differentiating between heel fat pad syndrome and plantar fasciitis can be done by pressing on specific areas of the heel. With heel fat pad syndrome, pressing on the middle of the heel is usually painful, while pressing closer to the inner edge, where the plantar fascia attaches, is more painful with plantar fasciitis. Diagnostic imaging, such as ultrasound or MRI scans, can provide more accurate differentiation between the two conditions.
Referred Pain from the Lower Back
Pain in the foot can also be caused by referred pain from the lower back. The sciatic nerve, which runs from the lower back down the leg, can become compressed or irritated, leading to pain that radiates into the foot. A healthcare professional can perform tests, such as the Slump Test, to determine if the sciatic nerve is involved in the pain. If lower back involvement is suspected, further evaluation and treatment may be necessary.
Plantar Fasciitis: Symptoms
The primary symptom of plantar fasciitis is heel pain, specifically in the bottom of the heel. The pain is often described as a stabbing or sharp sensation and is usually worse in the morning or after periods of inactivity. Some common symptoms of plantar fasciitis include:
It's important to note that while plantar fasciitis is a common cause of heel pain, there are other conditions that can cause similar symptoms. Therefore, it is crucial to consult a healthcare professional for an accurate diagnosis.
Causes of Plantar Fasciitis
Plantar fasciitis can have various causes, including:
It's important to address these underlying causes to prevent or manage plantar fasciitis effectively.
Treatment Options for Plantar Fasciitis
The treatment for plantar fasciitis aims to reduce pain, inflammation, and promote healing of the plantar fascia. Here are some common treatment options:
It's important to consult a healthcare professional to determine the most appropriate treatment plan for your specific condition.
Alternative Treatment Options
In addition to traditional treatment options, there are alternative therapies that may help with plantar fasciitis. These include:
These alternative treatments may be used in conjunction with traditional therapies or as standalone options, depending on the individual's preferences and healthcare provider's recommendations.
How to Prevent Plantar Fasciitis
Preventing plantar fasciitis involves taking steps to reduce the risk factors and stress on the plantar fascia. Here are some preventive measures:
By incorporating these preventive measures into your daily routine, you can reduce the likelihood of developing plantar fasciitis and calf pain.
Heel Spur Syndrome and Plantar Fasciitis Are Not the Same Thing
Heel spur syndrome and plantar fasciitis are often used interchangeably to describe the same condition. However, researchers suggest that these terms are oversimplified. Heel spur syndrome refers to the presence of a bony growth (heel spur) on the heel bone, while plantar fasciitis involves inflammation or irritation of the plantar fascia. Imaging studies often show a combination of factors, including bone edema, changes to the heel fat pad, injuries to the plantar fascia, and the presence of heel spurs. Therefore, it is more accurate to use the term "plantar heel pain" to describe the condition.
Frequently Asked Questions
Q: Can plantar fasciitis cause calf pain?
A: While calf pain is not a direct symptom of plantar fasciitis, it can be indirectly related due to the altered gait pattern caused by the heel pain. The pain from plantar fasciitis can lead to compensatory movements and strain on the calf, resulting in calf pain or tightness.
Q: Can plantar fasciitis cause ankle swelling?
A: No, plantar fasciitis does not typically cause ankle swelling. Swelling around the ankle is more likely to be caused by issues related to the ankle joint or tendons crossing it.
Q: What are some conditions that are often misdiagnosed as plantar fasciitis?
A: Some conditions that can be mistaken for plantar fasciitis include heel spur syndrome, stress fractures, Achilles tendonitis, tarsal tunnel syndrome, heel fat pad syndrome, and referred pain from the lower back. It's important to consult a healthcare professional for an accurate diagnosis.
Q: What are the treatment options for plantar fasciitis?
A: Treatment options for plantar fasciitis include rest and activity modification, stretching exercises, orthotic devices, physical therapy, non-steroidal anti-inflammatory drugs (NSAIDs), steroid injections, extracorporeal shockwave therapy (ESWT), and surgery in severe cases. Alternative treatments such as acupuncture, massage therapy, ultrasound therapy, cold therapy, and plantar fascia-specific exercises may also be beneficial.