

For thousands of runners in Calgary, lacing up and hitting the trails is more than just fitness; it’s a lifestyle. From early morning jogs along the Bow River Pathway to tackling the challenging inclines of Nose Hill Park, Calgary’s natural landscape is made for running. But with regular training comes the risk of wear, strain, and injury, especially to your feet. And that’s why an increasing number of runners are prioritizing regular podiatry visits as part of their health routine.
The repetitive impact of running places significant strain on your feet, ankles, and lower legs. Every time your foot strikes the ground, it absorbs a force several times your body weight. Over time, this can lead to:
Plantar fasciitis (inflammation of the foot’s arch support tissue)
Achilles tendinitis
Stress fractures
Heel and forefoot pain
Recurring blisters, corns, and calluses
Toenail injuries and fungal infections
While these issues may seem minor at first, left untreated, they can progress into chronic conditions that sideline your training.
A podiatrist isn’t just for injury treatment; it’s about proactive care and injury prevention. Here’s what makes regular podiatry check-ups an essential part of a runner’s wellness plan:
Early Detection of Problems
Routine visits allow podiatrists to spot biomechanical issues, overuse symptoms, or minor injuries before they become major problems.
Injury Prevention
A podiatrist can assess your running gait, foot alignment, and footwear to recommend adjustments or orthotics that reduce injury risk.
Custom Orthotics and Shoe Advice
Not all feet are created equal. A podiatrist can prescribe custom orthotics or suggest specific running shoes that better support your arches and reduce strain on joints.
Performance Enhancement
Pain-free, properly aligned feet improve stride efficiency, endurance, and overall running performance.
Calgary-Specific Foot Care
Running in Calgary comes with its own set of challenges: icy sidewalks in winter, uneven trails, and dry, cracked heels during the hot, dry summers. Local podiatrists know these seasonal hurdles well and can offer tailored advice and treatments to help you stay active and injury-free year-round.
If you run regularly, it’s smart to schedule a foot health assessment at least once a year. But you should book an appointment sooner if you experience:
Persistent foot, heel, or ankle pain
Swelling, redness, or tenderness after running
Numbness or tingling in your toes or feet
Recurrent blisters, nail damage, or calluses
A noticeable change in the shape or function of your feet
Even small foot issues can turn into serious problems if left untreated.
Your feet face enough strain out on the trails; you shouldn’t have to settle for generic care. A specialized foot clinic in Calgary offers targeted, experienced treatment that considers the unique needs of active, outdoor-loving locals.
Whether you’re chasing personal bests or enjoying casual weekend runs, proper foot care keeps you moving safely and comfortably.
Your feet are your foundation. Keep them healthy, strong, and pain-free with regular visits to our trusted podiatrist in Calgary. Prevent injuries, improve performance, and enjoy every step of your run from the first mile to the finish line.
Book your podiatry check-up today and give your feet the expert care they deserve.
Foot pain can greatly impact your daily life, making simple activities like walking uncomfortable and restricting mobility. While some discomfort may be short-term, ongoing pain could indicate underlying issues that need professional attention. In this article, we'll explore the common causes of foot pain, when to seek professional help, and the role of a foot care clinic in diagnosing and treating your symptoms.
Foot pain can arise from various factors, including structural issues and lifestyle choices. Some common causes are:
Bunions and Hammertoes: Bunions are painful bony bumps that form at the base of the big toe, while hammertoes cause toes to bend, leading to discomfort and difficulty finding appropriate shoes.
Flat Feet or High Arches: Both conditions can cause improper weight distribution across the foot, leading to pain when walking or standing for extended periods.
Tendinitis: Tendon inflammation, such as Achilles tendinitis, can cause pain at the back of the heel and is often linked to overuse or improper footwear.
Recognizing these symptoms can help you understand the source of your discomfort. If you're experiencing persistent pain, it may be time to consult a foot care clinic.
Not all foot pain requires a visit to a clinic, but certain signs indicate that professional care is necessary:
Swelling and Redness: Swelling, redness, or warmth may be signs of an infection or inflammatory condition, which requires immediate medical attention.
Difficulty Walking: Struggling to walk or bear weight on your foot can suggest structural issues or severe inflammation that needs professional treatment.
Changes in Shape: Deformities like bunions or hammertoes should be assessed early to prevent long-term complications.
Numbness or Tingling: Loss of sensation or abnormal feelings in the feet can indicate nerve problems that require further investigation.
If you experience any of these symptoms, it's important to visit a clinic for a diagnosis and a personalized treatment plan.
They specialize in diagnosing and treating a wide range of conditions. Here's what you can expect during your visit:
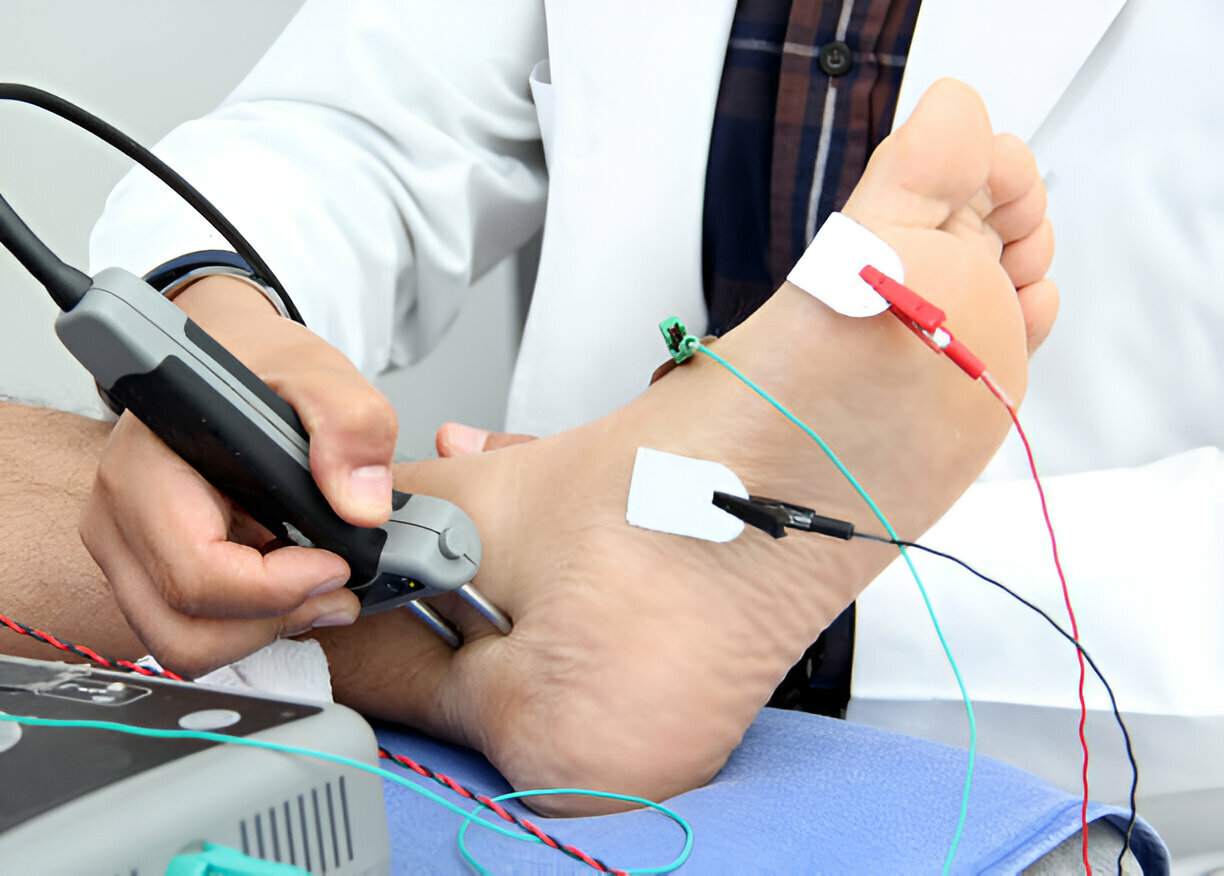
Advanced Diagnostic Techniques: Many clinics use tools like X-rays, ultrasound imaging, or 3D scanning to get a detailed look at your condition and ensure accurate diagnosis.
Personalized Treatment Plans: Based on your assessment, the specialist will create a treatment plan that may include orthotics, physical therapy, or medication. If necessary, they may refer you to a podiatrist for further care.
Prevention and Education: Clinics emphasize teaching patients how to prevent future problems through proper footwear, stretching exercises, and lifestyle modifications.
When you visit a foot care clinic, you'll have access to various treatment options tailored to your specific condition:
Custom Orthotics: These specially designed shoe inserts provide support and improve alignment to alleviate pain.
Physical Therapy: A physical therapist can create an exercise program to strengthen the muscles in your feet and improve flexibility.
Medication: Anti-inflammatory medications or corticosteroid injections may be used to manage pain and reduce inflammation.
Surgery: In severe cases, surgery may be required to address structural deformities or significant injuries.
Education: These clinics also provide education on maintaining foot health and preventing future issues, including advice on footwear and daily care routines.
Prevention is often more effective than treatment. Here are some tips to help maintain healthy feet:
Choose Proper Footwear: Invest in shoes that provide good support and fit well. Avoid wearing high heels or shoes that pinch your toes.
Practice Good Hygiene: Keep your feet clean and dry to avoid infections. Regularly check for changes like blisters, calluses, or discoloration.
Stay Active: Regular physical activity helps maintain a healthy weight and strengthens the muscles in your feet.
Stretch and Strengthen: Regularly stretch and exercise your feet and ankles to improve flexibility and prevent injuries.
Be Mindful of Activities: Ensure you warm up properly before exercise and wear the right footwear to prevent injuries.
By following these preventive measures, you can minimize the risk of pain and maintain the health of your feet.
Routine visits to a foot care clinic can significantly improve your overall health by:
Improved Mobility: Addressing pain allows you to move comfortably, leading to a more active and healthier lifestyle.
Holistic Health Management: Foot problems can be linked to other health conditions, such as diabetes or arthritis. Regular visits help manage these connections effectively.
Personalized Care: A clinic will provide a plan tailored to your unique needs, leading to better outcomes and satisfaction.
Education: Ongoing visits ensure you stay informed about foot health, empowering you to take proactive steps for long-term wellness.
When selecting a clinic, consider the following factors:
Range of Services: Choose the one that offers a comprehensive range of services, including diagnostic testing, treatment options, and rehabilitation.
Patient Reviews: Check online reviews or ask for recommendations to gauge patient satisfaction and care quality.
Convenience: Choose one that is convenient in terms of location and operating hours.
Insurance: Verify that it accepts your insurance or offers flexible payment plans.
By taking the time to do your research, you can ensure you receive the best possible care for your foot health.
Foot pain shouldn't limit your mobility or quality of life. Understanding the causes, knowing when to seek professional help, and utilizing the services of a foot care clinic are crucial steps toward achieving pain-free walking. If you're experiencing pain, don't wait. Visit a clinic to receive expert care and regain your comfort.
Take the First Step Toward Pain-Free Walking
Ready to walk pain-free? Contact our foot clinic in Calgary today to schedule your appointment and start your journey toward healthier feet and improved mobility!
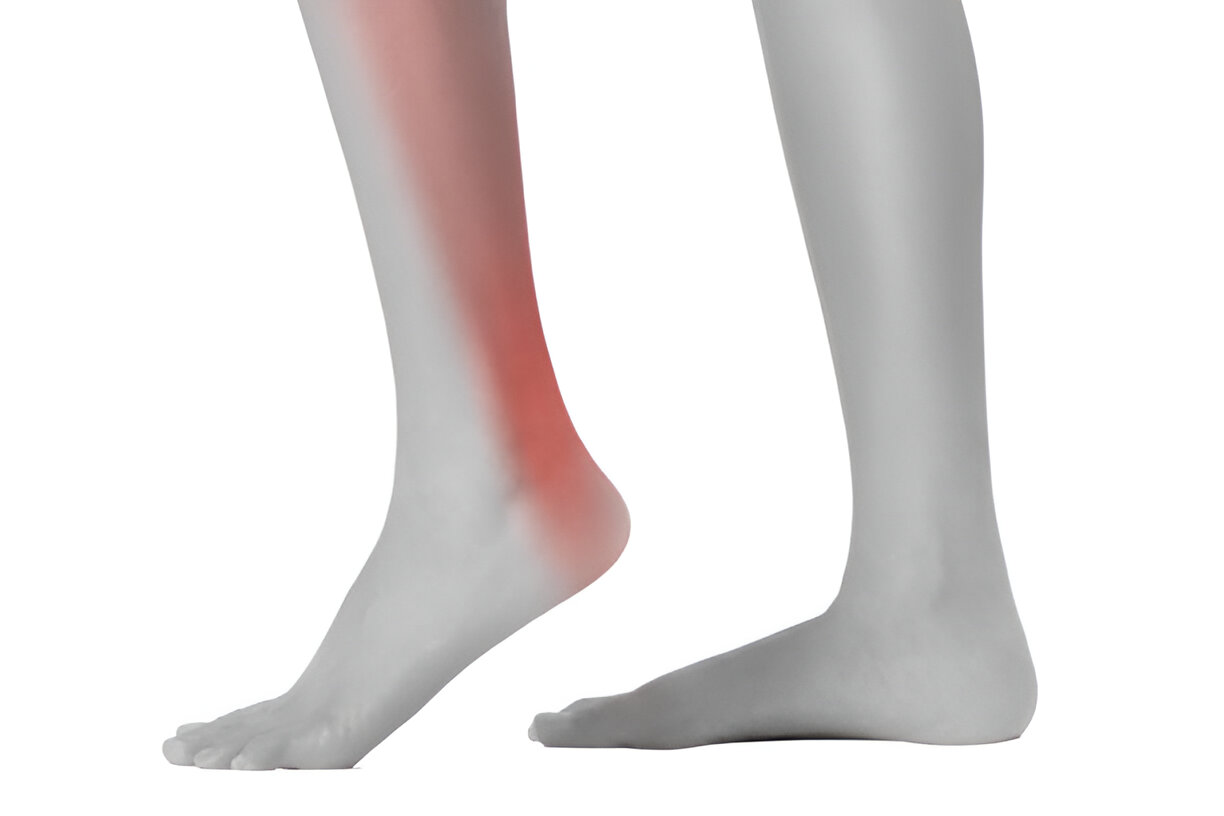
The Achilles tendon is the largest and strongest in the human body, connecting the calf muscles to the heel bone. Achilles tendonitis is a common overuse injury that occurs when this tendon becomes inflamed or degenerated. It is a painful condition that can significantly impact your mobility and quality of life if left untreated.
It develops gradually over time due to repetitive stress or strain on the tendon. It is commonly seen in athletes, particularly those participating in high-impact sports like running, jumping, or basketball. However, it can also affect less active individuals, especially as they age.
Several factors can contribute to the development of Achilles tendonitis, including:
Overuse and Overtraining: Engaging in excessive or high-intensity physical activity without adequate rest and recovery can strain the Achilles tendon, resulting in inflammation and degeneration.
Sudden Increase in Activity: Rapidly increasing the duration, frequency, or intensity of your physical activity, such as suddenly ramping up your running mileage or trying a new sport.
Improper Footwear: Wearing shoes with inadequate support or cushioning, or shoes that are worn out, can increase stress on the tendon during physical activity.
Biomechanical Factors: Structural issues such as flat feet, high arches, or leg length discrepancies can disrupt the body's natural weight and force distribution, increasing strain on the Achilles tendon.
Age: As you age, the Achilles tendon becomes less flexible and more prone to degeneration, increasing the risk.
Certain Medical Conditions: Conditions like rheumatoid arthritis, diabetes, or obesity can increase its risk by affecting the health and function of the tendon.
The primary symptoms of Achilles tendonitis include:
Pain and Discomfort: You may experience dull, aching pain along the back of the heel and lower leg, especially during or after physical activity.
Stiffness: The Achilles tendon may feel stiff, particularly in the morning or after periods of inactivity.
Swelling and Tenderness: The surrounding area may appear swollen and sensitive to the touch.
Decreased Range of Motion: You may have difficulty flexing or pointing your foot due to the pain and stiffness.
Weakness and Instability: The Achilles tendon may feel weaker, making it difficult to push off or bear weight on the affected leg.
Ignoring Achilles tendonitis can have serious consequences for your health and well-being. If left untreated, the condition can progress and lead to the following complications:
Chronic Pain and Discomfort: Persistent inflammation and degeneration can result in chronic, debilitating pain that interferes with your daily activities and quality of life.
Increased Risk of Rupture: The Achilles tendon can weaken over time, making it more prone to partial or complete tears serious and debilitating injuries that require surgery and a lengthy recovery period.
Altered Gait and Mobility: The pain and stiffness can cause you to alter your walking or running gait, potentially leading to further musculoskeletal problems, such as knee, hip, or back pain.
Reduced Physical Activity and Fitness: When left untreated, it can severely limit your ability to engage in physical activity, leading to a decline in overall fitness and cardiovascular health.
Increased Risk of Other Injuries: Compensating for the Achilles tendon injury by altering your movement patterns can increase the risk of developing other overuse injuries, such as plantar fasciitis.
Permanent Damage: If the condition progresses, it can undergo structural changes, including thickening, scarring, and calcification, potentially resulting in permanent impairment and loss of function.
Fortunately, Achilles tendonitis can be effectively treated with a combination of conservative and, in some cases, surgical interventions. The specific treatment approach will depend on the severity of your condition and the underlying cause. Common treatment options include:
Rest and Activity Modification: Reducing or temporarily stopping the activities that aggravate your problem can help reduce inflammation and allow healing.
Ice and Anti-Inflammatory Medications: Applying ice to the affected area and taking over-the-counter anti-inflammatory medications can help alleviate pain and swelling.
Stretching and Strengthening Exercises: Gentle stretching and targeted strengthening exercises can help improve flexibility, stability, and overall tendon health.
Orthotic Devices: Specialized shoe inserts or braces can help support the Achilles tendon and correct any underlying biomechanical issues.
Physical Therapy: A physical therapist can provide a comprehensive rehabilitation program, including manual therapy techniques, exercises, and other modalities to address the root causes.
Injection Therapy: In some cases, your healthcare provider may recommend corticosteroid or platelet-rich plasma (PRP) injections to help reduce inflammation and promote healing.
Surgery: If conservative treatments are unsuccessful, surgery may be necessary to repair or reconstruct the Achilles tendon in severe or chronic cases.
Ignoring Achilles tendonitis can have serious consequences, leading to chronic pain, reduced mobility, and an increased risk of more severe injuries. Early diagnosis and prompt treatment are crucial for preventing the progression of this condition and avoiding long-term complications.
By recognizing the causes, symptoms, and potential risks, you can take proactive measures to address the issue and protect your overall health and well-being. Remember, addressing the problem at the first signs of discomfort can help you avoid the more severe consequences and get you back to your active lifestyle as quickly as possible.
If you are experiencing persistent or worsening Achilles tendon pain, don't wait - schedule an appointment with us today. Early intervention can make all the difference in your recovery and long-term well-being.

Orthotics have become an increasingly popular solution for individuals dealing with various foot and ankle conditions. These custom-made inserts are designed to provide targeted support, alignment, and cushioning to alleviate pain and improve overall foot health. However, one common question that arises is, "How long do orthotics last?" In this comprehensive blog, we'll explore the factors that affect their longevity and provide you with valuable insights to ensure your investment in them lasts for years to come.
These are specialized devices that are custom-made to fit your feet. They are designed to address specific foot conditions, such as:
These custom-fitted inserts are typically made from various materials, including rigid plastics, soft foams, and even carbon fibre, depending on your individual needs and the condition being treated.
They work by providing targeted support, cushioning, and alignment to your feet. They can help to:
The lifespan of your orthotics can vary depending on several factors, including:
It's important to be aware of the signs that indicate these inserts may need to be replaced. These include:
If you notice any of these signs, it's best to consult with your foot care specialist to determine if it's time to replace them.
To extend the life of your orthotics, it's essential to follow proper care and maintenance practices. This includes:
By following these simple steps, you can help to ensure these inserts continue to provide the support and comfort you need for years to come.
Working with a reputable foot clinic can play a vital role in extending the life of your orthotics. Foot clinics can provide the following services:
By working with a reputable foot clinic, you can maximize their longevity and effectiveness, ultimately investing in the long-term health and well-being of your feet.
Orthotics can be a valuable tool in managing various foot and ankle conditions, but their longevity is not indefinite. By understanding the factors that affect their lifespan, following proper care and maintenance practices, and working with a reputable foot clinic, you can maximize the benefits of your investment in foot health.
Remember, the key to long-lasting orthotics is finding the right solution for your individual needs and working closely with your foot care specialist to ensure they continue to provide the support and comfort you require.
If you're in the Calgary area and looking for a reputable foot clinic in Calgary to help you find the perfect orthotics for your needs, consider scheduling a consultation with our team of experienced professionals. We'll work closely with you to create a customized solution that provides the long-lasting support and relief you deserve. Contact us today to take the first step toward optimal foot health.

Your feet are the foundation of your body, supporting your weight and enabling you to move freely. However, a variety of foot disorders can develop, ranging from minor irritations to severe conditions that can significantly impact your quality of life. Understanding these common problems and seeking professional help can help you maintain optimal foot health and prevent further complications.
Foot disorders can be complex and require specialized care. Visiting a foot clinic with experienced podiatrists can provide you with the necessary expertise to accurately diagnose your condition, develop an effective treatment plan, and prevent the worsening of your symptoms. By addressing these problems early on, you can avoid long-term complications and enjoy greater mobility and comfort.
1. Plantar Fasciitis: A condition characterized by inflammation of the thick band of tissue (plantar fascia) that runs along the bottom of your foot, often caused by overuse, poor foot mechanics, or improper footwear.
2. Bunions: A bony protrusion at the base of the big toe, typically caused by a genetic predisposition, improper footwear, or a biomechanical imbalance.
3. Hammertoes: A deformity where the toe joints bend downward, leading to the formation of a claw-like appearance, often caused by wearing ill-fitting shoes or an imbalance in the muscles.
4. Ingrown Toenails: A condition where the corner or side of the toenail grows into the surrounding skin, causing pain, swelling, and potential infection, commonly caused by improper nail trimming, tight-fitting shoes, or injury.
5. Heel Spurs: Bony growths on the underside of the heel bone, usually caused by repetitive stress or strain on the foot, such as from running, jumping, or standing for long periods.
6. Corns and Calluses: Thickened, hardened areas of skin that develop in response to excessive friction or pressure, often caused by ill-fitting shoes or abnormal mechanics.
7. Achilles Tendinitis: Inflammation of the Achilles tendon, the large tendon that connects the calf muscles to the heel bone, typically caused by overuse, improper training, or a sudden increase in physical activity.
8. Athlete's Foot: A fungal infection that causes itching, scaling, and redness between the toes, often contracted in warm, moist environments like public showers or pool areas.
9. Morton's Neuroma: A thickening of the nerve tissue between the toes, usually between the third and fourth toes, often caused by wearing high-heeled or narrow shoes that compress the toes.
10. Flat Feet (Pes Planus): A condition where the arches of the feet are either partially or completely collapsed, which can lead to pain, instability, and difficulty with certain physical activities, often caused by genetics, injury, or obesity.
The symptoms and signs of foot disorders can vary depending on the specific condition, but may include:
● Pain, swelling, or inflammation in the affected area
● Redness, warmth, or discoloration of the skin
● Changes in the shape or appearance of the foot or toes
● Difficulty walking or bearing weight on the affected foot
● Numbness, tingling, or burning sensations
● Decreased range of motion or flexibility in the foot or ankle
It's important to pay attention to any persistent or worsening discomfort and seek professional medical attention from a clinic to ensure proper diagnosis and treatment.
When you visit a foot clinic, the podiatrist will begin by conducting a thorough examination of your feet, which may include:
● Taking a medical history and discussing your symptoms
● Performing a physical examination to assess the affected area
● Ordering imaging tests, such as X-rays, MRI, or ultrasound, to obtain a clear diagnosis
Based on the findings, the podiatrist will develop a personalized treatment plan that may include:
● Conservative treatments, such as rest, ice, compression, and elevation (RICE)
● Medications to reduce inflammation or manage pain
● Custom orthotics or supportive devices to address biomechanical issues
● Physical therapy or exercises to improve strength and flexibility
● Surgical interventions, if necessary, to correct structural abnormalities or chronic conditions
The goal of the treatment plan is to alleviate your symptoms, restore function, and prevent the worsening or recurrence of the condition.
Podiatrists are medical professionals who specialize in the diagnosis, treatment, and prevention of foot and ankle conditions. They are trained to identify the underlying causes of problems and develop comprehensive treatment plans to address both the immediate symptoms and the long-term health of your feet.
At a foot clinic, a podiatrist can provide a wide range of services, including:
● Performing comprehensive examinations and assessments
● Diagnosing and treating disorders, such as those mentioned earlier
● Prescribing and fitting custom orthotics or supportive devices
● Administering injections or other conservative treatments
● Performing minimally invasive or surgical procedures, if necessary
● Providing guidance on proper care, footwear, and preventive measures
By working closely with a podiatrist at a foot clinic, you can ensure that your foot health is in good hands and take proactive steps to maintain optimal function.
Visiting a foot clinic can provide you with numerous benefits, including:
1. Accurate Diagnosis: The specialized expertise of a podiatrist can help ensure that your foot condition is properly identified, leading to more effective treatment.
2. Personalized Care: Foot clinics offer customized treatment plans tailored to your specific needs, taking into account your medical history, lifestyle, and goals.
3. Access to Advanced Treatments: Foot clinics often have access to the latest technologies and treatment options, allowing for more comprehensive and effective care.
4. Improved Mobility and Comfort: By addressing your problems, a foot clinic can help alleviate pain, improve your range of motion, and enhance your overall quality of life.
5. Preventive Care: Podiatrists can provide guidance on proper care, footwear selection, and exercises to help prevent the development or recurrence of disorders.
6. Convenience: Many foot clinics offer convenient scheduling and accessible locations, making it easier for you to prioritize your foot health.
Your feet are the foundation of your body, and taking care of them should be a priority. By understanding common foot disorders, recognizing the signs and symptoms, and seeking professional help from a clinic, you can take proactive steps to maintain your foot health and prevent long-term complications.
Remember, your feet play a crucial role in your overall well-being, and addressing any foot problems early on can have a significant impact on your quality of life. Don't hesitate to visit a clinic and work with a qualified podiatrist to develop a personalized plan for your foot health.
To schedule an appointment with a top-rated foot clinic in Calgary and take the first step towards optimal foot health, call us and schedule your appointment with our trusted podiatrists in Calgary, today!